Treatment Court work is challenging, interesting, and rewarding. However, recovery is a long road, and it can take a long time before participants start to see lasting changes, as they work to acquire essential knowledge and skills. This can be frustrating for everyone. Frankly, all that listening that treatment court programming requires can get a bit, well, boring. What’s the best way to “supercharge” that process? Decades of research supports the Chinese proverb “I hear I forget, I see I remember, I do, and I understand.” The more we can engage participants not just through their brains but through doing, the more likely they are to understand, assimilate, and integrate recovery skills and knowledge. It’s not complicated: “Would you show me how you did that…” “Let’s practice that together…” and “Can you stand up and do…” are the kinds of prompts that ALL members of the team can integrate into their interactions with participants. While therapists are generally tasked with teaching participants essential recovery knowledge and skills, the entire team is responsible for helping to keep those skills active, to provide opportunities for practice and feedback, and to offer encouragement. The payoff is substantial, as research shows that infusing action into our encounters with participants boosts the acquisition of knowledge and use of skills.
The negative impact of parental substance use on children’s well-being is well documented within the literature. Family Treatment Courts (FTCs) specifically aim to provide parents involved with the child welfare system with access to clinical treatment and recovery support services in an effort to enhance family functioning and help families stay together and thrive. However, a large percentage of participants in all types of treatment court programs have children (or serve in the role of parent/guardian). As a result, these participants could benefit from enhancing their knowledge and skills within the area of parenting.
Question: who should know about treatment courts? Answer: everyone, right? While everyone should know about the work and benefits of treatment courts, how we communicate with specific audiences – which we call stakeholders – must be tailored to their role, location, and function. This means that a message to a legislator inviting them to a drug court graduation would be different than a press release announcing the treatment court graduation to the media. The logistical information may be the same but the “so what?” varies across stakeholder groups. According to Ulmer, Sellnow and Seeger (2019), “To communicate more effectively, organizations must determine the types of communication relationships or partnerships they currently have with primary stakeholders.” How do you identify your relationships and partnerships? We can help with that. The NDCRC will be releasing “Marketing your Treatment Courts” in May for Treatment Court Month to help you tell the story of the work of treatment courts.
Statistics
Are you one of the 70 million people in the U.S who experience sleep problems? About one-third of adults get fewer than 7 hours of sleep and report symptoms of insomnia. About 10% of adults at any given time meet the criteria for insomnia disorder, reporting ongoing difficulty getting to sleep, staying asleep, and/or returning to sleep that results in problems with functioning. Another common sleep disorder is sleep apnea (about 10% of adults), in which the person stops and starts breathing again many times during sleep. Sleep apneas can lead to life threatening conditions and requires formal assessment and treatment by a medical provider. As we noted in the Beyond the Field article “
Sleep, Trauma and Substance Use,” quality sleep is key to overall health, emotional stability, planning, and sound decision-making. Poor sleep is associated with accidents, heightened pain sensitivity, unemployment, and mental health problems. For treatment court participants, sleep problems can interfere with recovery, making it more difficult to engage in treatment, maintain employment, and use skills to cope with psychiatric symptoms.
People with opiate use disorders (OUD) are at much higher risk of sleep impairments than the general population. Researchers report that as many as 84% of people with OUD experience significant sleep disturbances. Opiate use can create and perpetuate a harmful cycle, in which sleep problems and pain sensitivity trigger opiate use, and opiate use in turn leads to poor sleep and greater pain sensitivity – especially as withdrawal becomes part of the cycle. Furthermore, people with OUD are at much higher risk of not only obstructive sleep apnea, but central sleep apnea when the brain stops sending signals to the muscles that control breathing. This is a condition distinct from the immediate impact on respiration that can follow opiate administration. Studies indicate that about 40% of people with OUD have some form of sleep apnea – four times as many people in the general population. The relationship between OUD and sleep is complex: there are many factors that contribute to poor sleep among individuals with OUD, including co-occurring psychiatric disorders, financial stress, unstable housing, living in unsafe areas, a history of trauma, as well as the use of alcohol, nicotine and other drugs. (Dunn et al., 2018).
Do Medication Assisted Treatments Address Sleep Problems?
While the benefits of medication assisted treatments for OUD (MOUD) are well documented (SAMHSA, 2021), better sleep does not appear to be one of them. Research indicates that sleep does not improve with MOUD. A large study of individuals using methadone found that most reported moderate to severe sleep disturbance at the start of methadone treatment and that their disordered sleep persisted throughout treatment (Nordmann et al., 2016). Likewise, patients treated with buprenorphine did not fare any better in terms of improved sleep (Dunn et al., 2018). Again, the roots of sleep disturbance in OUD are complex. For individuals using both methadone and buprenorphine, psychiatric impairments were the strongest predictor of disordered sleep. Researchers are exploring the possibility that the medication itself causes some sleep problems or makes pre-existing sleep problems worse. MOUD is a critical component of OUD treatment, so it is important that treatment court team members are aware of how common sleep issues are among their participants and find ways to support them.
An Action Plan for Addressing Sleep Disturbance in OUD and MOUD
So, what can you do to assist participants experiencing disordered sleep? An important first step to addressing this issue is to increase awareness among all team members as to just how common disordered/dysregulated sleep is among individuals with OUD and receiving MOUD. Furthermore, team members should be knowledgeable about the relationship between poor sleep quality and some problematic behaviors (e.g., poor attendance, disengagement, forgetfulness, etc.) they observe among participants. It is important to note that individuals may not be aware that their sleep quality is poor nor that it is negatively impacting other aspects of their lives.
Below are relatively simple (and free) steps your treatment court team can take to bring this issue into the forefront of your work with participants.
1. As part of your enrollment/intake process, ask individuals about their sleep patterns.
- How many hours of sleep do you get each night (on average)? What time do you go to bed and wake up?
- Where do you sleep?
- Do you have trouble falling asleep? Do you have trouble waking up?
- On a scale of 1-5 (1=not at all rested to 5=very rested), how rested do you feel when you wake up?
2. In addition to asking individuals these questions in casual conversation, you can add an empirically validated screening tool to your enrollment/intake process. While not a comprehensive list, the below-listed screening tools are free and can be administered by non-clinicians:
Each of these tools includes a
scoring rubric which will determine if someone should be referred to a medical provider for a comprehensive medical assessment to rule out other high-risk conditions that may be affecting sleep (e.g., sleep apnea). When in doubt, refer an individual to a medical provider for an assessment as their condition could be life threatening.
3. It is also crucial for participants to know that disordered/dysregulated sleep is a very common experience among individuals with OUD and receiving MOUD. Once serious physiological/biological conditions have been ruled out by medical professionals, treatment court team members can and should normalize the realities of sleep dysfunction and work with participants to identify strategies that will assist in mitigating the negative side effects associated with poor sleep. Moreover, it’s important that treatment court team members reaffirm the benefits of MOUD and together with the below-listed suggestions, sleep may improve over time and recovery will continue.
Below are several prompts that can be used by any member of the treatment court team. For example, a case manager during a case management session, probation officer during a reporting meeting, peer recovery support specialist during 1-1 interactions, or a judge during the court review session.
- Ask about the environment and other protective factors: “I know you’ve been having sleep problems. Can we help you talk to your family/roommates about that so they can support you? How can we support you in getting safer/more stable housing?”
- Urge treatment for mental health challenges: “I hope you are getting help for problems like stress and depression and trauma – that can also help with sleep. And vice versa. Can we help you get the treatment you need?”
- Help them use cognitive reminders to assist with everyday tasks that may be negatively impacted by lack of sleep: “It’s easy to forget what you’re doing if you haven’t had good sleep. Let’s review how a planner or calendar can help you stay organized? You can set reminders on your phone. I can help show you how to use one…”
- Encourage them to decrease nicotine and alcohol use: “You wouldn’t think so, but tobacco, e-cigarettes, and alcohol can really mess with sleep. Is that something you want to think about or change?”
- Ask about how they engage in physical activity: “I know how hard it is to get good sleep too. Walking during lunch has really helped. What sorts of physical activity do you engage in? When could you incorporate physical activity into your weekly schedule?”
- Ask if clients are using any mindfulness apps or working on relaxation in therapy. “So, mindfulness and breathing differently really help some people relax and fall asleep. Have you talked about that with your counselor?”
- Free, evidence-based apps such as iBreathe may be helpful.
- Help clients develop a structured daily schedule that includes sleep. It will vary depending on employment (e.g., 3rd shift will be different from 2nd shift); parenting or other caregiving, etc.
- Ask about how they can make their sleeping space and bedtime routine more supportive of sleep: “Can you control the lighting or noise level where you sleep? Can you put away your phone a half hour before bedtime?”
- Offer cognitive behavior therapy for insomnia (CBT-i) as part of your menu of evidence-based treatment. Some of the above activities above are covered in more depth in CBT-i.
- The U.S. Department of Veteran’s Affairs (VA) has developed CBT-i Coach, a free app that supplements healthcare treatment but can be used on its own https://mobile.va.gov/app/cbt-i-coach
Call to action:
Discussing disordered/dysregulated sleep is not practicing medicine. All members of the treatment court team should normalize disordered/dysregulated sleep, work to increase knowledge in this area, and actively work to support participants experiencing this issue.
Your treatment court team can take several steps to improving the program’s capacity to address the needs of participants. To this end, we would offer the following suggestions for specific action steps you can take:
- Identify at least one medical doctor in your area with whom your team can refer individuals in need of routine medical exams, assessments for specific conditions, etc.
- Identify at least one pharmacist in your area with whom you can consult regarding medication interactions and general questions regarding medications.
- Build a relationship with a medical and/or pharmacy school in your area. Medical/pharmacy students could observe your treatment court planning and court sessions, as well as provide consultation.
This is the fifth in our Beyond the Field series of articles that explore trauma and its impact on treatment court work. Treatment court participants can face challenges including complex health problems, poverty, discrimination, substance use, trauma, just to name a few. As a result, poor sleep may not rise to the top of the list of issues to address with individuals. Yet sleep disturbances underlie many of the physical, cognitive, and emotional struggles that can derail recovery. Over 80% of people who have been diagnosed with post-traumatic stress disorder (PTSD) also have a sleep disorder, and adding substance use to the mix compounds sleep problems exponentially (Vandrey et al. 2014). Recognizing and targeting sleep problems as one dimension of treatment could not only improve health and well-being but may be key to helping people more fully engage in treatment court activities.
What are sleep disorders?
Sleep is essential to our ability to regulate our mood, make wise decisions, avoid accidents, encode and retrieve memories, and learn new things. Treatment court clients are expected to do all these tasks, and not doing so impedes their progress to graduation and blocks long-term recovery. Not all difficulties with sleep meet criteria for a sleep disorder, but sleep disorders affect people with PTSD at much higher rates than the general population. The most common sleep disorder is insomnia, which includes problems with falling asleep, staying asleep, and returning to sleep after waking. Other sleep disorders that commonly occur with trauma are nightmares and obstructive sleep apnea (Coloven et al., 2018).
How are sleep, trauma, and substance use related?
The relationship between substance use and sleep problems is fairly well studied, and treatment court practitioners and providers should be aware of the importance of addressing sleep problems within the process of recovery. Use of stimulants, alcohol, opiates (e.g., too much sleep and insomnia rebound), and marijuana withdrawal all can cause or exacerbate sleep disturbance. The self-medication hypothesis is well supported as well, as people who struggle with sleep may turn to substances to help. Much more research is needed to determine best treatment practices, and the Substance Abuse and Mental Health Services Administration has published a useful resource to learn more (SAMHSA, 2014; https://store.samhsa.gov/sites/default/files/d7/priv/sma14-4859.pdf)
The impact of trauma on sleep is powerful. Re-experiencing traumatic events often occurs in the form of nightmares, and people become hypervigilant, or intensely on guard against future dangers. Depending on the nature of the trauma, people may have come to associate nighttime, darkness, and sleepiness with extreme vulnerability. We are never more defenseless than when asleep, and people who have experienced trauma form negative expectations and cognitions related to the inevitability of future harms.
There is growing evidence that PTSD, substance use disorders, and sleep disorders are bi-directionally linked (Vandrey et al. 2014).
For example, disordered sleep can make people more susceptible to trauma (e.g. accidents) and more likely to use substances to help them sleep; people with PTSD have symptoms that directly interfere with sleep (e.g. nightmares), and may misuse substances to get relief from both; and people who use or are withdrawing from substances find their sleep is disturbed and can experience heightened PTSD symptoms. Substance use offers quick relief from their distress, but then withdrawal from the same substances leads to sleep disturbance. These are just a sample of the dynamic relationships among these factors, but more research is needed to understand the interplay among them and find effective treatments to address all three factors in concert.
Assessing sleep problems
Whether an individual reports “trouble sleeping” or has a diagnosable sleep disorder, it is important for providers to assess sleep disturbances. While parasomnias (e.g., sleepwalking) and obstructive sleep disordered breathing may require specialists and technologies (e.g., polysomnography) to diagnose, there are validated self-report measures of insomnia that can identify triggers in order to promote use of coping skills direct sleep interventions (see Colvonen, et al. 2018). Sleep diaries are another tool that asks the individual to track their own sleep, recording bedtimes, wake times, sleep latency, night awakenings and total amount of sleep. The data collected can inform not only diagnoses but provide a road map for developing treatment plans. As sleep disturbances do not occur in a vacuum, it is essential also assess trauma symptoms and substance use at the same time.
Treatment of sleep disorders as they co-occur with trauma and substance use
Research shows that treatment of trauma does not necessarily lead to improved sleep, and the same is true for treatment of substance use. Identifying and addressing sleep problems early in treatment may provide several benefits for people with trauma. Since disordered sleep is widely accepted as a common problem, providers may focus on sleep as a “foot in the door” to express empathy for their distress and begin the winding therapeutic pathway forward toward.
Pharmacological interventions can be effective in treating sleep disorders, however there is a risk of misuse that should be considered. Obstructive sleep apnea, narcolepsy, parasomnias, and restless leg syndrome need to be addressed by specialists and generally are not relieved by talk therapies alone. Non-pharmacological therapeutic interventions, at least for insomnia, have been found to be more effective than medications in people with PTSD and substance use disorders (SAMHSA 2014; Colvonen et al., 2018; Vandrey et al., 2014).
Cognitive behavioral therapy for insomnia (CBT-I), is a brief (6-8 sessions) approach comprised of well-supported behavioral interventions like restricting sleep, stimulus control, such as structuring the environment to be more conducive to quality sleep. It also integrates cognitive therapies that target negative thoughts about sleep and other dysfunctional beliefs that interfere with sleep. The approach is heavily researched and is endorsed by the Department of Veteran’s Affairs (VA) and the American College of Physicians as a first line of treatment for insomnia-even as it co-occurs with PTSD. The manualized intervention can be administered with individuals or groups, and there are mobile technologies such as apps that supplement in-person treatment (e.g., the VA’s CBT-i Coach). Imagery Rehearsal Therapy, or IRT has shown promise in the treatment of nightmares in PTSD. A cognitive therapy, IRT involves “re-writing” of recurrent nightmares to make them less distressing and repeatedly imagining and rehearsing the new scenarios to make them less potent (Colvonen et al., 2018).
What Treatment Courts Can Do
- Assure that the whole team is educated about the complex relationship among mental health, substance use disorders and sleep.
- Ask participants about sleep troubles and have empathy for some of their cognitive and emotional struggles in this context.
- Locate and contract with providers who are trained to assess sleep disorders and who can offer non-pharmacological, cognitive, and behavioral treatments. Although online programs and self-help books have been shown to help, the complexity of co-occurring disorders and treatment court clients are at high risk, high need symptoms.
- Don’t expect sleep to get better just because mental health symptoms and/or substance use improves. Consider offering treatment for sleep, especially insomnia, separately but as an integrated part of treatment for other mental health and/or substance use disorders. If all treatments are not integrated, there is a real risk of playing a winless game of “Whack-a-Mole.”
- At minimum, offer participants sleep hygiene information as part of their health and self-care and recovery services. While this information may not fully address many of the complexities of the trauma-substance use-sleep disorder cycle, sleep hygiene skills overlap and reinforce other skills participants are already learning in treatment, including mindfulness, relaxation training, exercise, and changing self-talk to be more accurate and self-compassionate.
Improving sleep in treatment court participants can potentially impact the cognitive, emotional and physical impairments that interfere with recovery. Participants could engage more fully in treatments for PTSD and other mental health struggles, as well as substance use interventions, improving the chances of successful recovery.
Perhaps you have heard these common misconceptions about trauma therapy for treatment court participants:
- Trauma therapies are too harsh ”they could relapse and they won’t graduate.
- Better to treat the substance use first, THEN address the trauma.
- Whatever trauma-focused therapy is available, that will be good enough.
- It is expensive (for providers) to learn trauma-focused therapies, and they are too complicated.
The National Drug Court Resource Center provides free resources to enable treatment courts to implement evidence-based practices and maximize the effectiveness of their programs. In this fourth article in our series on trauma-informed practices, we provide a brief overview of trauma-specific treatments that have the most scientific support, why these therapies are a good fit for many treatment court participants with trauma, and ways to facilitate greater access to these effective treatments.
Importance of integrating treatment for PTSD and substance use treatment
It is well known that trauma and substance use disorders co-occur at very high rates, and treatment courts are well positioned to provide treatment for both, concurrently. This integrated model offers outcomes that are far superior to the outdated, sequential approach that requires treating substance use disorder first, THEN the trauma (Flanagan et al., 2016). Integrated treatment allows clients to address PTSD symptoms that are directly linked to substance use, and vice versa. A sequential model that focuses on treating substance use first reduces the chances that trauma will ever be addressed before the treatment court participant either drops out or completes the program. Providers may fear that clients with PTSD are too fragile in that encouraging clients to face their trauma memories and intense emotions directly could lead to relapse or dropping out of treatment. Conversely, treatment court participants have greater supports and structure in place than in any other time in their lives, so treatment courts are encouraged to take advantage of this window of opportunity.
Trauma-focused therapies with the best outcomes
The following trauma-focused treatments have been rigorously studied and are recommended/strongly recommended by the American Psychological Association and the U.S. Department of Defense (Veterans Services). All are fairly brief (8-16 sessions), and share a direct focus on exposure to memories of the trauma. Some also emphasize changing clients maladaptive beliefs about the trauma and themselves. All the approaches involve temporary discomfort, as distressing memories are activated through exposure (imagined or real-life) and processed in a structured, systematic manner under the direction of the therapist (Watkins et al., 2018). Decisions about which treatment approach is the best fit will depend on nature of the trauma (e.g., combat-related, victim of sexual assault, witness to a violent event), the complexity of the trauma, client preference, and realistically, availability of clinical providers who offer the intervention.
Cognitive Processing Therapy (CPT).People who have experienced trauma try to make sense of the occurrence and can develop distorted beliefs about themselves and the trauma. These stuck points can keep the individual from healing, and include beliefs such as I have myself to blame and as long as I trust no one, I will be safer. Treatment extends over 12 sessions and involves activating the traumatic memory, which includes writing and reading a narrative account of the trauma. At the same time, the therapist helps the client to identify the maladaptive cognitions associated with the traumatic event and shift them to become more accurate and helpful (Resick, Monson & Chard, 2017).
Prolonged Exposure (PE).After educating the patient about the nature of PTSD and how PE works, the therapist uses exposure to both imagined and real-life situations, as well as people and places associated with the clients unique trauma. After repeated exposures, the client ultimately learns that the feared (avoided) consequence will not occur and is able to move forward and use more adaptive coping strategies as opposed to avoidance. The therapy typically takes 8“15 sessions (e.g., Foa et al, 2007).
Trauma-focused Cognitive Behavior Therapy (TFCBT). Many have heard of this as an evidence-based therapy for children. However, adults also benefit from the integration of behavioral (e.g., imaginal exposure to the distressing memory) and cognitive components. Clients learn to identify triggers of re-experiencing, practice discriminating between then vs. now, identify and dispute dysfunctional thoughts, as well as reshape beliefs about themselves, the trauma, and the world.
Eye Movement Desensitization Reprocessing (EMDR). In this treatment the therapist utilities exposure to the traumatic memory, coupled with eye movements (left and right) and sometimes tapping and sounds. EMDR differs from the other recommended approaches in that cognitions are not explored, exposure to the distressing memory is briefer, and there is no assigned homework. The therapy typically takes 6-12 sessions (Shapiro, 2017).
These therapies have been found to be very effective for people who are actively using substances, have thoughts of suicide (but low intent), are unhoused, or have minimal education. There are a few exclusions. Trauma specific treatment is not recommended for people who currently have unmedicated mania or psychosis, or who are at current high-risk for suicide, or who require immediate detoxification services.
Who should receive these therapies?
First, assessment of trauma symptoms is critical. Treatment court participants may not report or display trauma symptoms at the initial screening and assessment for admission to treatment court, as they may have normalized their experiences or may not be ready to disclose such sensitive information. However, members of the treatment court team should be on alert for signs of trauma and refer participants to trauma therapy providers for assessment. Providers should routinely assess participants for PTSD and continue to assess throughout treatment.
When working with justice-involved individuals with SUD or COD, SAMHSA (2015) recommends the use of the following trauma screening instruments:
PTSD Checklist for DSM-5 (PCL-5)
and
Select 1 of the following publicly available resources:
Similarly, SAMHSA (2015) recommends the use of one of the following trauma assessment instruments, which should be administered by a licensed clinician:
How available are trauma specific therapies to treatment court participants?
There are few studies on the use of trauma therapies in treatment court populations, and more work needs to be done to assess barriers to access as well as mental health and substance use outcomes. Veterans Treatment Courts (VTCs) are likely to be more familiar with and offer trauma specific therapies. The U.S. Veterans Administration has been a leader in funding the development, research, training and dissemination of these interventions. The therapies are applicable to non-veteran populations, and clinicians are encouraged to receive training to provide these interventions. All approaches are related to aspects of cognitive and behavior therapies, and most providers should already be familiar with the theories and be able to utilize the therapy manuals, handouts, and free phone apps for patients (e.g. PE Coach and CPT Coach).
Treatment Courts are encouraged to pursue training for providers in these strongly recommended trauma-specific approaches and to utilize the free and low-cost resources below to learn more.
This is the third in a series of articles regarding trauma-informed treatment courts. In December 2021, we offered an overview of SAMHSAs (2015) six principles of trauma-informed care and evidence-based strategies for the screening and assessment of trauma in participants. In January 2022, we explored literature on trauma-informed spaces and courtrooms and reviewed findings from environmental psychology. In this edition of Beyond the Field, we review work related to trauma-informed drug testing as it relates to the trauma-informed principles of safety, trust and transparency, collaboration and mutuality, empowerment/voice & choice, peer support, and cultural, racial/ethnic and gender needs.
According to Best Practice Standard #7, Drug and alcohol testing provides an accurate, timely, and comprehensive assessment of unauthorized substance use throughout participants enrollment in the Drug Court (NADCP, 2018, 26). Treatment court teams use drug/alcohol results to monitor participants use of substances to make decisions regarding appropriate treatment services, supervision levels, and the administration of both incentives and sanctions. To this end, the success of any Drug Court will depend, in part, on the reliable monitoring of substance use (NADCP, 2018, 27). Given the vital role of drug/alcohol testing plays within the treatment court environment and the frequency with which participants engage in this program activity (minimum of twice per week during first few months of enrollment is best practice), it is vital that testing protocols are trauma-informed and do not undermine other aspects of the program.
Review of trauma and its associated symptoms. SAMHSA defines trauma as resulting from an event, series of events, or a set of circumstances that is experienced by an individual as physically or emotionally harmful or life-threatening and that has lasting adverse effects on the individuals functioning and mental, psychological, social, emotional or spiritual well-being (2014). Because trauma is common among treatment court participants, teams will want to take action to minimize its negative impact on engagement in services, communication, problem-solving, decision making, and outcomes.
Symptoms of Posttraumatic Stress Disorder (PTSD) and related Acute Stress Disorder (ASD) include the following four clusters (American Psychiatric Association, 2013):
a) Re-experiencing the traumatic event, or having intrusive, recurring memories or dreams related to the event. Places, sounds, lighting, thoughts, objects, and even words can trigger re-experiencing.
b) Avoidance of situations, thoughts and feelings related to the event. Avoidance symptoms can cause people to resist instructions or escape to safety.
c) Disturbance in arousal and reactivity. People may be easily startled, on edge, irritable, or become angry or aggressive. They may have trouble focusing, sleeping, and paradoxically, may engage in risky or destructive behavior.
d) Numbing and/or other changes in cognition and mood. Numbing, emotional withdrawal or shutdown when triggered, negative thoughts, self-blame, feelings of isolation and apathy are common.
You can probably picture participants who exhibit these behaviors, but might not have considered them to be trauma-related reactions. Trauma-informed courts recognize that the people, places and things embedded in everyday treatment court operations can trigger and exacerbate PTSD and ASD, or even re-traumatize participants. They respond by altering policies and practices to minimize these risks, often at low or no costs.
The where, who and how of trauma-informed drug testing.
The National Center on Substance Abuse and Child Welfare (NCSACW) conducted a trauma-informed care assessment project, or walkthrough process, with five sites across the country (NCSACW, 2015). The site visits of child welfare, substance use treatment centers, and family treatment courts identified several common trauma triggers, including drug testing spaces and procedures. Restrooms tended to be noisy, uncomfortable, and located in high-traffic areas with little or no privacy.
The information and examples are wisely organized by the principles of trauma-informed care.
Some highlights include:
Safety
- Give participants written AND verbal information about what to expect during a UDS each time a screen is required
- Have signage available in the restroom such as where to place the sample, when it is OK to flush and wash hands. Do not rush.
- Close off restroom when in use and be sure it is clean and free of hazards
- Ensure alternative means of testing, e.g. mouth swabs
Trust and Transparency
- Inform participants and provide documentation explaining why the UDS is being conducted, and when/how participants can access results
- Allow participants to observe the sample being closed and labelled
- Ensure participants know who to contact if they have questions, complaints or want to follow-up
Collaboration and Mutuality
- Provide a checklist of options about decisions they can make (if available) regarding use of a hat, whether or not they want to have conversation or quiet, soft music, or have water running.
- The tip sheet provides a sample information sheet that along with the above options, lists the purpose, substances tested for, and includes the statements “We understand this can be an uncomfortable process and want you to feel as safe as possible
- Provide a way for participants to offer feedback.
Empowerment, Voice & Choice
- Give participants a choice of which trained staff is giving the UDS.
- Ensure participants are aware of their rights as a service user, and provide in writing
- Avoid stigmatizing language dirty UA).
Peer Support & Mutual Self-help
- If peer support is requested during the UA, ensure this option is available.
Culture, Gender & History
- Require staff to participate in trauma-informed care, cultural humility, and equity training as part of onboarding process.
- Ensure UDS staff represent the population being served.
- Ensure easy access to menstrual products.
The UDS tips provided by Trauma Informed Oregon are not particularly expensive or difficult to implement, but they do require leadership and consistency. Drug/alcohol testing is a key component of the drug treatment court model and can/should be conducted with an eye toward minimizing the potentially traumatizing effects on participants. Treatment court teams should examine current policies and procedures and make necessary modifications where appropriate. Ensuring that all aspects of treatment court programs are trauma-informed will improve participant retention rates and increase the likelihood of participant success.
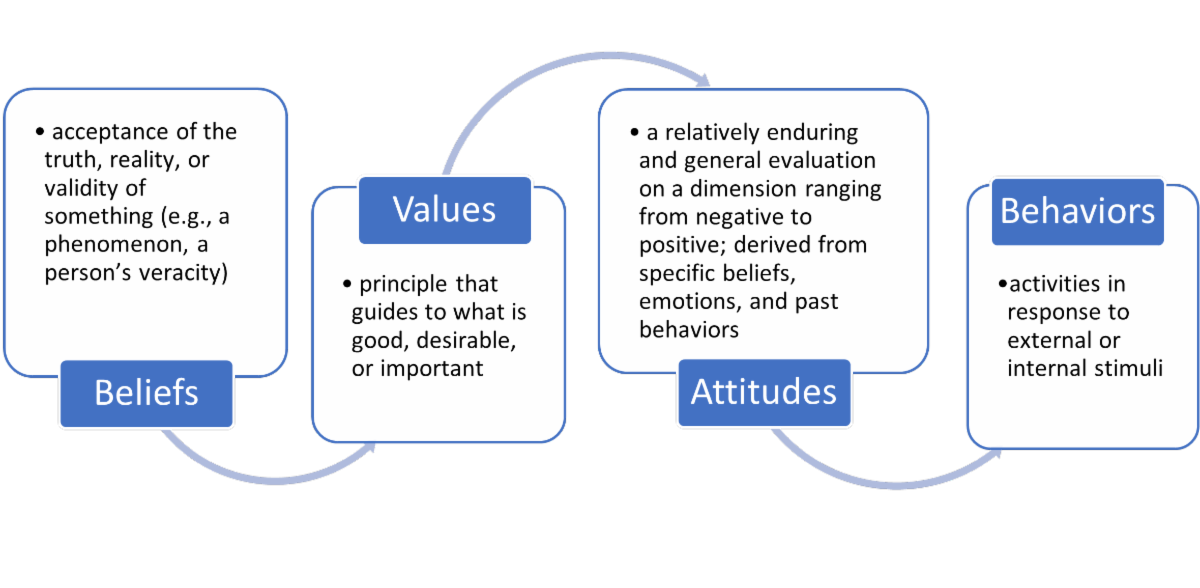
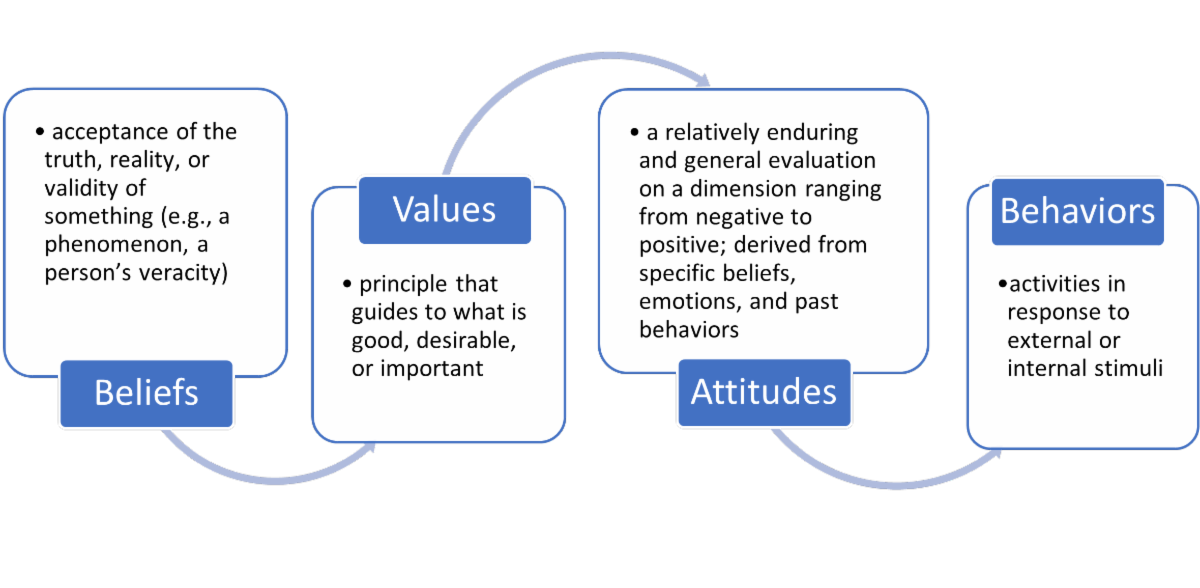
Connection is a through-line in the operating philosophy of therapeutic jurisprudence. Yet, the anatomy of connection and that of therapeutic jurisprudence is complex, and precise roadmaps for either are debated among scholars. However, perhaps a helpful framing to best work toward living out this philosophy is to consider four elements: beliefs, values, attitudes, and behaviors.
In the last article, the concept of mindfulness was introduced and defined as paying attention to what is happening in this moment, without judgement or reactivity to the thoughts, feelings, and physical sensations that arise (Kabat-Zinn, 1994). As we untangle the anatomy of therapeutic jurisprudence and connection, mindfulness practice allows you to notice what is happening in your mind and body. What thoughts, feelings, and sensations arise when you agree with an idea? When you disagree? Feel bored? When you dislike the idea, have unpleasant feelings, or uncover a judgment of yourself? The foundational skill of mindfulness invites you to stay curious about whatever comes up for you. Curiosity can make way for you to be kind towards yourself and “importantly “ persistent in examining and reflecting upon the ideas ahead.
In unpacking the anatomy of connection and therapeutic jurisprudence, we will first focus on the role of beliefs.
Psychologists define beliefs as the acceptance of the truth, reality, or validity of something, particularly in the absence of substantiation (APA, 2022). Before we examine the role of beliefs in treatment court work, we must first familiarize ourselves with our own thoughts that are pertinent. You are invited to consider the following questions carefully and honestly:
- What thoughts arise when I think about people involved in the treatment court system?
- It may be helpful to consider your ideas about their motivation, wants, needs, behaviors, capacity for / interest in change, etc.
- What thoughts arise when I think about treatment courts?
- It may be helpful to consider your ideas about their purpose, design, utility, approach, effectiveness, etc.
- What thoughts arise when I think about my role in the treatment court system?
- It may be helpful to consider your ideas about your knowledge, skills, preparedness, attitude, motivation, capacity to provide support / make change, desire to help, resources, etc.
Now that you have begun unfolding your own thoughts, we will outline beliefs that therapeutic jurisprudence invites practitioners to try on in treatment court work. These beliefs can include:
- What do we believe about people involved in the treatment court system?
- All people have strengths, gifts, and talents.
- People are not their circumstances, conditions, experiences, or choices. People are in circumstances, experience conditions, have experiences, and make choices.
- People have a complex life story we know only a fraction about. It may include but is not limited to their involvement in the justice system.
- People have needs and wants as well as hopes for their lives.
- People are complex, and understanding them takes time, energy, and interest.
- People can change.
- People deserve support in their efforts to change.
- People will naturally make mistakes in the process of attempting to change their lives.
- All people regardless of identity or circumstance deserve to be treated with dignity and respect.
- All people regardless of race, ethnicity, gender, sexual orientation, sexual identity, physical or mental disability, religion, or socioeconomic status deserve the same opportunities as other individuals to participate and succeed in treatment courts.
- What do we believe about treatment courts?
- The law can be leveraged to have a therapeutic effect, resulting in psychologically healthy outcomes.
- A collaborative, non-adversarial approach is most effective to supporting people to change their lives.
- Building relationships is necessary to positively impact treatment and court outcomes.
- The opportunity for alcohol and other drug treatment and mental health services can make a meaningful difference in peoples lives.
- What do we believe about practitioners roles in the treatment court system?
- The treatment court system works best with a connected, collaborative team.
- All members can learn from one another.
- All members of the multidisciplinary team bring a unique, necessary perspective and play an important role in participant outcomes.
- Transitioning to a team approach from an adversarial approach can take time, patience, and intention.
Why might honestly examining your own thoughts matter? Are your thoughts your actual beliefs? When do these automatic thoughts arise? Are the thoughts you had consistent with the beliefs outlined above? Where did your thoughts come from, and how might you challenge those that are inconsistent with those connected to therapeutic jurisprudence? Under what circumstances might your thoughts shift? (e.g., when you witness positive change, when your mood is low, when your body is activated, when your stress level is high, when youre feeling really energized, etc.) And, when are you most generous thoughts about yourself around when are the least generous ones pleasant?
Our beliefs about ourselves, others, and the world around us are deeply connected to our values, shape our attitudes, and influence our behavior”both personally and professionally.
In this way, we cannot solely focus on practitioners behaviors in cultivating a healthy, effective workforce. Yet, thoughts are not beliefs”unless we decide so.
We need to consider all aspects of the anatomy of therapeutic jurisprudence, starting with our actual beliefs about ourselves, others, and the work itself. Exploring our own thoughts means examining how we arrived at the ideas we have and the openness to challenges the ideas we hold. A part of the process also involves considering how our thoughts may automatically become beliefs without consciousness might affect our treatment of others.
Using the 5 As of mindfulness, you can distinguish thoughts from beliefs and uncover your actual beliefs with intentionality“ a process that is critical to engaging skillfully and effectively in your work. For example, imagine you have thoughts that label those with whom you work as offenders and criminals. In using mindfulness, the following could unfold:
- Attention: intentional focus to the present moment:
- Noticing the labels of offender and criminal in your mind and conversations with colleagues
- Noticing judgmental thoughts about actions and choices of those involved in the treatment court system
- Noticing feelings of frustration, ambivalence, and an urge to disengage from helping
- Noticing sensations of agitation in the body
- Acceptance: recognition of the truth of what is happening in the mind and body (note: this is not resignation, simply acknowledging what is true at this time):
- This is just what is happening right now “ judgmental thoughts, frustrated feelings, and the urge to disengage.
- Allowance: making space for the full experience of what is happening without pushing it away (unless it is skillful in the moment to have such boundaries)
- giving permission for what is happening in the mind and to exist”taking a moment to breath and avoid busyness that is sometimes deigned to move us away from what is really happening
- Attitude: bringing qualities of curiosity, non-judgment, openness, and kindness to witnessing and holding the inner experience
- Its interesting Im having these thoughts; Its understandable to have these thoughts “ because Im feeling extra stressed today, and this is the language that I hear all the time in society, too. All emotions are normal to feel.
- Action: choosing deliberative responses (rather than automatic, habitual reactions) that are grounded in awareness of the present moment
- Reminding yourself that thoughts arent facts and do not have to be representative of your actual beliefs because they arose in your mind. Our beliefs are our choices.
- Reminding yourself that labels like offender and criminal are reductionistic, diminishing of someones humanity, and disconnecting; they are problematic because they label the entire person by a behavior and make us feel far and separate from that person (i.e., disconnected)
- Choosing to reframe that language in your mind in speech”maybe even by simply thinking about the person by their name, dropping the label altogether. (i.e., Sam experienced a substance use relapse versus An offender in the program relapsed.)
- Taking care of yourself in the best way for you in response to the frustration/agitation that is around and possibly connected to automaticity of labeling (e.g., talking with a supervisor about a challenging interaction with the person)
- Taking a step to reconnect to that person, even if only in your mind and body (e.g., think of one thing you have in common with that person)
Thoughts are only mental experiences that we often mistake as facts or chosen beliefs; however, we can choose to buy into our thoughts or not. Beliefs are, in fact, choices. Bringing more consciousness to the ways in which with think about ourselves, others, and work positions us to stay connected”to ourselves, to others, and to our professional values, attitudes, and behaviors.
What we choose to believe directly impacts how we engage. How we engage directly impacts the lives of others.
And, we want to engage with the belief that those in the treatment court system are, in fact, criminals, offenders, participants people.
A Connection Call to Action:
This week, you are invited to engage in a connection call to action to try out the ideas discussed.
Connecting with yourself:
Examine your beliefs about yourself, focusing on your strengths. Take a few moments each day to make a list of 5 of the strengths you demonstrate in your work.
Connecting with others:
Examine your beliefs about those in a participant role, focusing on identifying their strengths. Take a few moments each day to make a list of 5 of the strengths you see in a person with whom you are/were working. Each day, choose a new person to think about. You are especially encouraged to focus on those people who brought up feelings of frustration for you or with whom you have/had a strained working relationship.
In the introduction to the series, the role of connection to ourselves and others was offered as an essential practice to live out the philosophy of therapeutic jurisprudence that underpins treatment courts. But, how do we stay connected to ourselves and others?
Connection requires us to make conscious choices. Active listening, asking questions for understanding, and identifying a participant’s strengths are all examples of choices that can help us stay in connection with others. What keeps us from making these choices? How do we notice when we are in connection, and how do we sustain it? How do we notice when disconnection happens, and then, how do we take steps to reconnect?
The answers to these questions—and ultimately making deliberate choices—first relies on our capacity to notice what is happening in the mind and body. The quality of that noticing—how we do the noticing—is also important to balancing both effective communication with others and taking care of ourselves. The skill that supports us in this is called mindfulness.
What is Mindfulness? (And, What It is Not)
Mindfulness is paying attention to what is happening in this moment, without judgement or reaction to the thoughts, feelings, and physical sensations that arise (Kabat-Zinn, 1994). The practice invites us to adopt an attitude of openness and curiosity about what we are experiencing, with kindness towards ourselves, so that we are able to respond, versus react, to not only what is happening in us but also around us in the environment.
Said another way, mindfulness involves five A’s: attention, acceptance, allowance, attitude, and action (Lee, 2020, 2021):
- Attention: intentional focus to the present moment
- Acceptance: recognition of the truth of what is happening in the mind and body (note: this is not resignation, simply acknowledging what is true at this time)
- Allowance: making space for the full experience of what is happening without pushing it away (unless it is skillful in the moment to have such boundaries)
- Attitude: bringing qualities of curiosity, non-judgment, openness, and kindness to witnessing and holding the inner experience
- Action: choosing deliberative responses (rather than automatic, habitual reactions) that are grounded in awareness of the present moment
Discussion of mindfulness is increasing culturally, which has resulted in the increased accessibility of learning and practicing opportunities. Yet, with the rise of attention to the practice comes, at times, misconceptions. These misconceptions include:
- Mindfulness is about escaping, emptiness, zoning out, or “nothingness.” In actuality, mindfulness is about “falling awake” to the life that you are actually living, versus escaping, numbing, or erasing parts of it (Kabat-Zinn, 2018). Instead, mindfulness is the gentle noticing and befriending of all of the thoughts, feelings, and sensations that make up our inner world.
- Mindfulness is “woo-woo” and is only useful for certain people. Mindfulness is not woo-woo; it is a tradition that spans thousands of years and a variety of traditions. Over the past 40 years, a vast body of research has emerged and bares out the benefits of mindfulness-based interventions for wellbeing in a number of ways, including related to common experiences such anxiety, depression, and chronic pain (Khoury, Sharma, Rush, & Fournier, 2015). Mindfulness has been introduced in healthcare, clinical, educational, business, and legal settings to explore its usefulness; and research shows benefits for both clinical and non-clinical populations (Visted, Vøllestad, Nielsen, & Nielsen, 2015). The vast majority of people can potentially benefit from paying attention to their experience without judgement and with kindness, and the scientific community continues to explore mindfulness-based interventions.
- Mindfulness involves having a blank mind and no thoughts. The mind wanders, and this is completely natural—even during formal mindfulness practices like meditation. The practice of mindfulness is actually about the steady, consistent practice of bringing the attention back to the present moment when we’re lost in or overidentified with thinking. Overidentification is when we merge with our thinking in such a way that we don’t recognize thinking is happening. For example: “I am a terrible worker” is an example of being fused with a thought. A more mindful approach would be the observation “I am having the thought ‘I am a terrible worker.’” This observational stance can be incredibly helpful de-intensifying the impact of that thinking. Observation creates a pause that makes space for the awareness that thoughts aren’t facts.
- Mindfulness requires you to meditate. Formal meditation is the practice of concentrating on an “object;” examples can be the breath, sounds, thoughts, the body, or even the entire field of whatever arises in awareness. Formal meditation is an incredibly helpful approach to support your capacity to practice mindfulness in everyday moments of living. However, formal meditation is only one mindfulness practice. Any activity can actually be engaged in mindfully—driving a car, walking down the hallway, giving a friend a hug, or brushing your teeth. Bringing non-judgmental attention to any moment is a practice that is always available to us.
- Mindfulness will erase stress and discomfort. While it is true that the practice of mindfulness may at times result in less stress or discomfort, mindfulness is not centered around “arriving” to any particular state of being (e.g., calm, stress-free, happy), though arguably the practice does cultivate a greater overall sense of wellbeing over time. The practice is truly about being with whatever is here, which paradoxically can, in fact, help us experience the transient nature of all thoughts, feelings, and sensations. Yet, it is helpful to avoid beginning a mindfulness practice attached to particular outcomes; such an expectation to lead you to think you’re “doing it wrong,” if certain experiences are not different. Mindfulness will not erase stress and discomfort; mindfulness will support you having a different relationship with stress and discomfort.
- Mindfulness is a “cure-all.” Though the practice has become increasingly popular in various settings, it is important to note that mindfulness is not a panacea, and further research is needed to better understand where, how, and with whom it can be most helpful. While there is strong evidence to support its use, certain practices may be unhelpful or in need of modification if someone is experiencing certain symptomology (e.g., trauma symptoms). More research is needed about the mindfulness-based interventions and certain populations or mental health concerns (e.g., schizophrenia) in service of prioritizing safety and effectiveness with those with whom we are working. Facilitators of mindfulness-based interventions also do need to be trained in the intervention, and education about trauma-sensitive mindfulness practice is helpful regardless of the nature of the intervention (i.e., clinical or non-clinical).
Why Mindfulness?
Research suggests we spend approximately 50% of our time lost in thoughts about the past or future (Killingsworth, Gilbert, D. T. (2010) instead of the moment-to-moment experience we are having.
Consider the consequences of not paying attention to at least half of the moments in your life.
- What does that mean for how much energy you have to create the life you want?
- What does that mean for your wellbeing?
- What does that mean for your relationships?
- What does that mean for how you engage in your work?
- What does that mean for staying in connection with those you serve in your work?
While practicing mindfulness does not guarantee a particular “state” of being, noticing our experience with kindness and without judgement does position us to make more conscious choices. Those choices, if intentional, can better embody our values, meet our needs, reflect our knowledge, and allow us to exercise our skillsets.
So, What Could Mindfulness Look Like at Work?
We can practice mindfulness using formal practices (e.g., meditation) or informally through everyday activities. The purpose of formal practice is actually to support us carrying over what is learned to everyday life, both in personal and professional contexts. Everyday activities could include, for example, drinking your coffee in the morning at your desk. Using all your senses to bring you to the here-and-now, you may take time to notice its color, smell its richness, hear any noise it may make moving in the cup, and experience it through touch and taste when taking a slow sip. And, you can practice mindfulness when you interact with others.
Consider the following scenario: a participant has missed three sessions of a group treatment program you are running. What could be some of the automatic, habitual thoughts, feelings, and sensations that arise for you?
Let us say the following was your experience:
Thought: He doesn’t event care. So disrespectful. Why do I even try? I’m tired of working harder than he is.
Feeling: frustration
Sensations: heat in the body, increased heart rate
Now consider what reactivity to this internal experience might look like, remembering reactivity is not intentional, deliberate behavior but rather more automatic and habitual reactions.
Reactivity might look like:
Reactivity: assuming your thoughts are “true,” complaining to a coworker about the participant, being short the next time you see the participant, or failing to see the participant’s strengths due to ruminating on the “disrespectful” behavior
Were we to consider taking a mindfulness approach, how might you relate to the experience of the thoughts, feelings, and sensations outlined above? This might look like:
- Attention: intentional focus to the present moment:
- “I am having the thoughts that ‘He doesn’t event care. So disrespectful. Why do I even try? I’m tired of working harder than he is.’ I notice I feel frustrated. I can sense heat in my body and my heart rate rising.”
- Acceptance: recognition of the truth of what is happening in the mind and body (note: this is not resignation, simply acknowledging what is true at this time):
- I don’t like it, but judgement, frustration, and internal heat really is around for me right now.
- Allowance: making space for the full experience of what is happening without pushing it away (unless it is skillful in the moment to have such boundaries)
- giving permission for judgmental thoughts, the frustrated feeling, and the bodily sensations to exist; letting them be here instead of trying to push them away through distraction or busyness
- Attitude: bringing qualities of curiosity, non-judgment, openness, and kindness to witnessing and holding the inner experience
- “It’s interesting I’m having these thoughts;” remembering judgment, frustration, and an activated physiological response are all normal; noticing with as much kindness towards yourself as you can
- Action: choosing deliberative responses (rather than automatic, habitual reactions) that are grounded in awareness of the present moment
- deliberative responses such as taking a short walk before interacting with anyone, reminding yourself you do not have all of the information about the participant’s absences, reminding yourself of the participant’s strengths and the difficulty of the change process for all of us, active listening and asking questions to see understanding when meeting with the participant.
Certainly, many factors influence our automatic, thoughts, feelings, and sensations in response to the world around us. Perhaps our mood is low that day, we were just in an argument with a loved one two days before, the participant reminds us of a friend with whom we have a challenging relationship, or we have a pattern of interpreting participants’ absences as disrespectful to us personally—just as some examples.
No matter the explanation, we will experience automatic, habitual thoughts, feelings, and sensations. The key to being able to stay in connection with ourselves is to not abandon the experience we are really having. Connection with ourselves positions us to be able to take care of ourselves.
The key to being able to stay in connection with others is also not to abandon the experience we are having. Connection with others position us to make connective deliberate choices like listening, asking questions, and displaying empathy.
There is no greater sign of respect, no deeper signal of appreciation, no better gift than you can give yourself or others than you attention.
Each article in the Connection: The Essential Practice for Therapeutic Jurisprudence in Treatment Courts series will conclude by offering two features: Connection Questions to
Consider and Connection Calls to Action.
Connection Questions to Consider:
- When are you most mindful at work? What helps that to happen?
- When are you least mindful? What gets in the way?
- When in your day could you commit to pausing for a short meditation? (e.g., when you first sit down to your desk, when transitioning between meetings, before potentially stressful interactions)
A Connection Call to Action:
This week, you are invited to engage in a connection call to action to try out using mindfulness practice to connect with yourself and others.
- Connecting with yourself:
- Engage in 5 minutes of formal meditation per day. If you are new to meditation, guidance is very helpful. A wealth of free resources exist online, and you can also choose to explore guided meditations using apps (e.g., Waking Up, Headspace, Calm).
- Engage in an “everyday practice” of mindfulness per day. Choose an activity that you regularly do—brushing your teeth, walking the dog, washing the dishes, etc. As best you can, try to notice the experience of the activity (versus thinking about the activity), choosing to anchor your attention on physical sensations. When the mind wanders, as it will, gently escort your attention back to the body. Use your senses to connect to the raw, direct sensations of the experience.
- Connecting with others:
- Choose one conversation per day to practice mindfulness. You do not need to mention you’re practicing to the other person. As best you can, focus your attention on the other person—what is being said, their body language, the emotional tone of what is shared. Notice when thoughts arise (e.g., planning what you want to say), and gently bring your attention back to the speaker. When you notice a thought, you might practicing “noting;” that is, simply saying to yourself “thinking,” which helps to avoid getting lost in the narrative the mind if creating. After noting, return to listening when the other is talking. Practice pausing and considering your words carefully.
By design, the judicial system wields disconnection as a tool to gain compliance, police behavior, and execute punishment. Rules are standardized, personal histories often remain unconsidered, change is sought through punitive means, and people are, quite literally, numbers. Arguably, the dehumanization inherent in this approach perpetuates, at least in part, the very social problems it seeks to address.
As a movement, the treatment court model is itself an answer to the ineffectiveness of disconnection in promoting behavioral change for those who experience challenges with substance use and/or mental health. The philosophy of therapeutic jurisprudence, which underpins the treatment court model, emphasizes the potential for psychologically healthy outcomes when the legal system is structured as a “restorative, remedial, and healing instrument” (ISTJ, 2022; Kawalek, 2020, p. 2; Stobbs, 2019). Therapeutic jurisprudence is concerned with “the human effects of the law” and the promotion of practices to benefit the “emotional, psychological, physical, relational, economic, and social personhood” of participants (Kawalek, 2020, p. 1-2). Treatment courts offer an important opportunity to leverage the legal system to make meaningful changes in people’s lives.
Collaboration is perhaps the hallmark of treatment courts. In identifying best practices, the National Association of Drug Court Professionals (NADCP, 2018b) emphasizes the importance of an interdisciplinary approach as well as complementary treatment and social services. Best practice standards also underscore the need for predictability, fairness, consistency, and evidenced-based principles for behavior modification in the operations of treatment courts—practices that cannot be actualized without both interdisciplinary and professional-participant collaboration. The NADCP standards further acknowledge the critical nature of attention to equity and inclusion for participant success; addressing historical patterns of discrimination and inequity certainly requires sincere collaboration (NADCP, 2018a).
The thread of collaboration can be traced back even further to NADCP’s earlier efforts to outline key components of treatment courts. NADCP names the “non-adversarial approach” as crucial to encourage collaborative, coordinated efforts to support participants (NADCP, 2004, p. 3). Another essential component is “ongoing judicial interaction with each treatment court participant,” a standard that explicitly highlights the need for an “active, supervising relationship” in service of increasing the likelihood of participant success (NADCP, 2004, p. 15). Emphasis is placed on early engagement with participants, interdisciplinarity, and “forging partnerships among treatment courts, public agencies, and community-based organizations” (NADCP, 2004, p. 23).
Without question, intentional, focused, collaborative relationships are central to the mission of the treatment court model, and such meaningful collaboration requires connection.
While scholars within psychology offer various conceptualization, social connection may be simply described as a sense of belonging, which can be derived from the experience of acceptance, concern, empathy, and care (Seppala, Rossomando, Doty, 2013). Arguably, a uniqueness of the treatment court model is the opportunity for social connection including
between participants and direct service providers (e.g., case managers, therapists), participants and others professionals (e.g., defense counsel, probation authorities, judges), as well as among the entire team of professionals collaborating with the participant. Notable to the treatment court approach is another, albeit a less obvious, opportunity for connection for participants—connection with self. That is, mental health service provision as well as case management services offer participants pathways to cultivating a sense of belonging to oneself through self-acceptance as well as concern, empathy, and care for the self. Lastly, treatment court professionals benefit greatly from being in connection with the self, too, which is helpful for both their own wellbeing and positioning them to be present and skillful in working with participants.
Connection—whether it be with self, others, or larger systems—is the nexus of change.
When participants are connected with themselves, they are best positioned to understand the influence of the past upon the present, identify their needs and values, establish goals, and take meaningful, congruent choices to shape their lives. The connection between professionals and participants results in participants feeling seen, heard, understood, and supported—often catalysts to personal growth and change. A treatment court team member’s own capacity to stay in connection with oneself results in the ability to embody professional values, utilize knowledge from their training, and effectively engage with participants. Further, professionals do not operate in a vacuum; connected collaborations, systems, and institutions result in stronger collaborations, systems, and institutions. The practices, processes, and policies of these larger entities matter—they can either reflect an investment in connection or disconnection. The ultimate goal of the treatment court model is to reduce recidivism through substance use and/or mental health treatment, and the means by which this goal is achieved is, in fact, staying in connection—perhaps the most essential, yet most unrecognized, practice necessitated by the treatment court model philosophy.
If connection is the birthplace of behavioral change, five primary questions emerge:
- How can treatment court practitioners stay in connection with themselves to be able to engage with participants skillfully?
- How can treatment court practitioners stay in connection with participants?
- How can treatment court practitioners support participants to stay in connection with themselves?
- What does a connected treatment court team look like? How can connection be cultivated and reflected in practices, processes, and policies?
- What does a connected criminal justice system look like? How can connection be cultivated and reflected in practices, processes, and policies?
In the Connection series, we will examine these questions as to untangle the rewarding, nuanced, and challenging aspects of working in treatment courts.
When you go into a court you don’t know what’s going on because you’re terrified. There are guns, they’ve got you chained up, and you’re under the influence. All these things are happening at once. — Trauma Survivor (SAMHSA et al., 2013).
People who have experienced trauma can be easily and suddenly overwhelmed, hypersensitive to sounds, confined spaces and objects. They may reflexively respond to these as life-threatening and can’t attend to or remember essential court proceeding or treatment-related information.
The field of Environmental Psychology studies how the physical environment, such as building design, floorplans, signage, and other features of buildings impact our behavior. Designs that provide privacy and a sense of safety are ideally suited for people who have experienced trauma (Garcia, 2020).
Of course, few courts, probation departments, treatment providers, etc. have the luxury of designing their own buildings. However, SAMHSA and other collaborators (2013) compiled tips for treatment court professionals that can help prevent or offset negative impacts of these often-intimidating spaces and promote a sense of safety and respect in participants. They highlight aspects of the physical environment that treatment courts can consider without great expense or delay.
Does your courtroom have seating that provides easy access to aisles and exits? If not, can seats be reserved near aisles? Where does the judge sit? DO they loom above the court, making eye contact and respectful connection difficult? Are people placed in handcuffs and shackled where all in attendance can see? Are the bathrooms where drug tests take place well lit? Is there a space where people can get some privacy if they need a space to calm down? Is the signage posted respectful? OR does it just instruct people what NOT to do?
The article provides a
table that describes potential triggers in the environment, the possible reactions of a trauma survivor, and a more trauma-informed approach that treatment courts may take. According to Garcia (2020), “The goal of trauma-informed design is to create environments that promote a sense of calm, safety, dignity, empowerment, and well-being for all occupants. These outcomes can be achieved by adapting spatial layout, thoughtful furniture choices, visual interest, light and color, art, and biophilic design.” It would behoove treatment court teams to assess the physical spaces where participants engage in program-related activities with a critical eye toward minimizing trauma.
Which clients in your treatment court have a history of trauma? How can you find out? Why does it matter? While the conversation about the prevalence and devastating effects of trauma has become increasingly open in justice settings, many treatment courts may be blind to it in their own programs or simply hope that good intentions will prevent further trauma. Perhaps now is the time to self-reflect as a treatment court and to take small, but meaningful actions right now.
According to SAMHSA, “Individual trauma results from an event, series of events, or a set of circumstances that is experienced by an individual as physically or emotionally harmful or life threatening and that has lasting adverse effects on the individual’s functioning and mental, physical, social, emotional, or spiritual well-being, (2014a, p. 7).” Trauma experiences can diminish the ability of treatment court participants to engage in programs and long-term recovery. So, what does it mean for organizations to be trauma-informed? First, in order for treatment court programs to fully embody a trauma-informed system of care, all program staff must:
1. Have a basic realization of the origins of trauma and the impact this can have on individuals, families, groups, and communities.
2. Be able to recognize the signs of trauma in individuals.
3. Continuously assess the ways in which policies, procedures, and practices should be revised in order to allow staff to respond to individuals appropriately.
4. Resist engaging in action(s) that may result in re-traumatization.
In addition, SAMHSA (2014a) identifies six key principles that should serve as the foundation for developing your trauma-informed systems of care.
1. Safety (this is #1 for a reason) – above all else, participants’ physical & emotional safety should be promoted in all settings & through all interactions. Individuals (i.e., staff and participants) who do not feel safe will not fully engage.
2. Trustworthiness & Transparency – treatment court operations should be transparent and conducted with an eye toward developing and maintaining mutual trust between and among stakeholders and participants.
3. Peer Support – incorporating peer recovery support specialists into your treatment court program is an effective way for individuals with lived experience to assist participants in their recovery.
4. Collaboration & Mutuality – recognizing and acknowledging that all treatment court team members and participants have unique roles/responsibilities is key to developing collaborative relationships based on mutuality and respect.
5. Empowerment, Voice, & Choice – treatment court team members look for opportunities to empower participants to make decisions and have a voice in their recovery.
6. Cultural, Historical, & Gender Issues – the treatment court program provides participants with access to clinical and recovery support services that are responsive to their cultural, racial/ethnic, and gender needs.
A good place to start moving toward being a trauma-informed treatment court is to screen participants for trauma exposure to determine which individuals are in need of a more thorough assessment and trauma-specific services. Several screening and assessment tools have been validated with justice-involved populations; a sample list is attached. This is by no means an exhaustive list, and note that separate tools have been developed for youth (Collaborative for Change, 2016) and adults (SAMHSA, 2015). Many of these tools are free, while some charge a nominal fee.
To conduct a screen sensitively that will yield valid responses, it is recommended that programs “take the time to prepare and explain the screening and assessment process to the client gives him or her a greater sense of control and safety over the assessment process.” (SAMHSA, 2014b, p. 94). Be prepared to reassess individuals as they grow more willing to disclose information over time.
In the coming months, Beyond the Field entries will periodically highlight literature on trauma-informed practices for different components of treatment courts, including drug testing, courtroom set-up and structure, team dynamics, use of language, and providing participants opportunities to have a voice and make choices.
Associating the word “brand” with treatment courts may seem to be a mismatch. Taking a closer look at what branding is, however, opens up possibilities for how we talk about the work of treatment courts with professionals, clients, and the larger community. In communication studies and rhetoric, one of the most prominent scholars who explains narratives and story is Walter Fisher. According to Stache (2017), “In 1978, Walter Fisher proposed a theory of narrative communication, which advances the idea that humans inherently tell stories and like to have stories told to them.” The idea of branding and brands comes from this human need for stories. In the commercial, business-to-consumer sense, brands function as a way for humans to create relationships with consumer goods (Twitchell, 2004). We sometimes call these “brand narratives.” Organizations tell stories in order to gain their stakeholders’ attention and every communication interaction between an organization with its audiences has an impact. In addition, Fisher explains that stories ideally have narrative coherence and narrative fidelity. Narrative coherence means that the story makes sense, and narrative fidelity means that the story rings true to the audience’s experience (Stache, 2017).
What does this look like for treatment courts? It means that the responsibility for communication falls on every member of the treatment court team, because every interaction is an opportunity to create a new reality – a new story – that builds on the mission and vision of your program. Does this mean every interaction must be perfect? Of course not. That’s neither realistic nor human. However, it does mean that open, honest, and authentic communication that aligns with a program’s mission and purpose can create a strong brand story. This strong brand story also means that the inevitable messiness of human communication happens within the context of a coherent story with fidelity. The process of developing your program’s brand can also build goodwill and trust with your intended audience, which will serve you well in times of both crisis and celebration.
Innovations like NADCP’s Equity and Inclusion Tool make it easier for treatment courts to “Do Better” to determine if their policies and procedures reduce racial, ethnic, and cultural disparities. But what about therapies? Are evidence-based interventions, say motivational interviewing (MI), equally relevant and effective for diverse populations?
No. The field has been slow to address this problem, but researchers have attempted to adapt existing, effective therapies to make them relevant for diverse clients. For example, Karen Chen Osilla and colleagues developed a web-based MI intervention in English and Spanish to improve the outcomes of Latino first-time DUI clients, (Osilla et al., 2012). They used a strategy called formative iterative evaluation, a multistep process, to assure the MI intervention content and delivery were responsive to linguistic and cultural needs.
First, MI researchers and health literacy experts for Latino & Spanish populations created an in-person MI intervention tailored to first-time DUI clients. Next, they conducted focus groups with clinicians and clients to determine what changes were needed. Then, they adapted the in-person MI intervention to an interactive web format in both English and Spanish. Finally, they tested it again to gather more feedback about its usability and cultural fit.
The developers made changes, such as translating idioms (“getting high”) and adding examples of ways that drinking could negatively affect family and friends. They integrated feedback on social and family values-related themes, adding “drinking with friends” as a reason to drink, “being a good role model” as a reason to stop drinking, and “not meeting family responsibilities or disappointing family/children” as negative consequences of drinking (p. 197). At the final test of the web-based format, clients who spoke only Spanish (compared to English-only and bilingual clients) “reported feeling less embarrassment, shame and discomfort with the web-MI” (p.199).
A later study of the intervention found it was likely not long or intensive enough to make a lasting impact, at least on its own. However, the study provides a sound example of a systematic, collaborative approach to developing effective multicultural therapies. Clearly, treatment court staff and providers cannot afford to wait for intervention research to catch up with the demand for culturally relevant therapies. In the meantime, we can remember that treatments are not “one-size fits-all,” and ask clients–especially those from diverse backgrounds–whether they feel respected, a sense of belonging, and if the therapy is actually helping, throughout their treatment court experience.
The NADCP Adult Drug Court Best Practice Standards champion the use of evidence-based practices, based on the best available research. While research can tell us what models and interventions work, the how of their delivery is less often discussed. The most effective treatment court teams go beyond the “what” of their program’s offerings (evidence-based practices) and relate to participants in ways that support and promote recovery (evidence-based relationships).
A Task Force on Evidence-Based Relationships was formed by the American Psychological Association to analyze the best available research to identify the core components of effective therapy relationships (Norcross & Wampole, 2011). The Task Force concluded that the therapeutic alliance, empathy, and gathering client feedback are clearly linked to positive outcomes. The therapeutic alliance entails mutually agreed upon goals, agreed upon tasks, and a sense of collaboration and relational bond between the two parties. Multiple rigorous studies also indicate that therapists who can express empathy (understand and acknowledge the client’s perspective) and who actively monitor client’s perceptions and responses to treatment are more effective. Relationship behaviors deemed ineffective and potentially harmful include a confrontational style, therapist comments that are hostile or blaming, judging the person versus their behavior, and applying a one-size-fits-all approach that ignores individual and cultural differences.
Relevance to Treatment Courts
While most members of treatment court teams are not therapists, the Task Force’s findings detail what works and doesn’t work in relationships that target lasting personal change. The following can apply to every court team role:
- To enhance the relational alliance, treatment court team members should frequently discuss participants’ personal values and motivations, and collaboratively review program and client expectations.
- While these relationships must remain professional, expressing genuine caring for participants can help form bonds that are healthy, respectful and meaningful.
- Directly asking clients for feedback about the program and their experiences provides opportunities to improve collaboration, to modify approaches as needed, and prevent premature termination.
- Confrontation has historically been a problem in the addictions field. Interactions that are infused with motivational enhancement elements, such as rolling with resistance, reflective responding and active listening serve as antidotes to these all-too-human, but toxic reactions.
- Individualized treatment plans that consider the individual’s unique and diverse identities are a hallmark of treatment court Best Practices, and the Task Force’s findings confirm this. “Fair treatment” does not equal “identical treatment.” It means tailoring the program and services to match the evolving needs of each individual.
Treatment court involvement is essentially a series of human interactions, so relationships between participants and the team are central to recovery. Substance use and criminal behavior can be viewed as rooted in disturbed relationships, disconnection and alienation, and treatment court professionals have the opportunity to make lasting impacts–not only via evidence-based techniques and operational models–but through meaningful, evidence-based connections.